The science, the promise, and the pitfalls
The idea of a “metabolic reset” has gained traction across wellness media, social platforms, and weight management programmes. The premise is appealing: that metabolism can be “retrained” or “rebooted” through short-term dietary changes, leading to improved fat loss, better blood sugar control, and renewed energy.
But what does the Metabolic Reset Diet actually involve? Is metabolism something that can truly be reset? And where does the science end and marketing begin?
This article explores the core principles of metabolic reset diets, the potential benefits, the risks, and what current metabolic research really tells us.
What is the Metabolic Reset Diet?
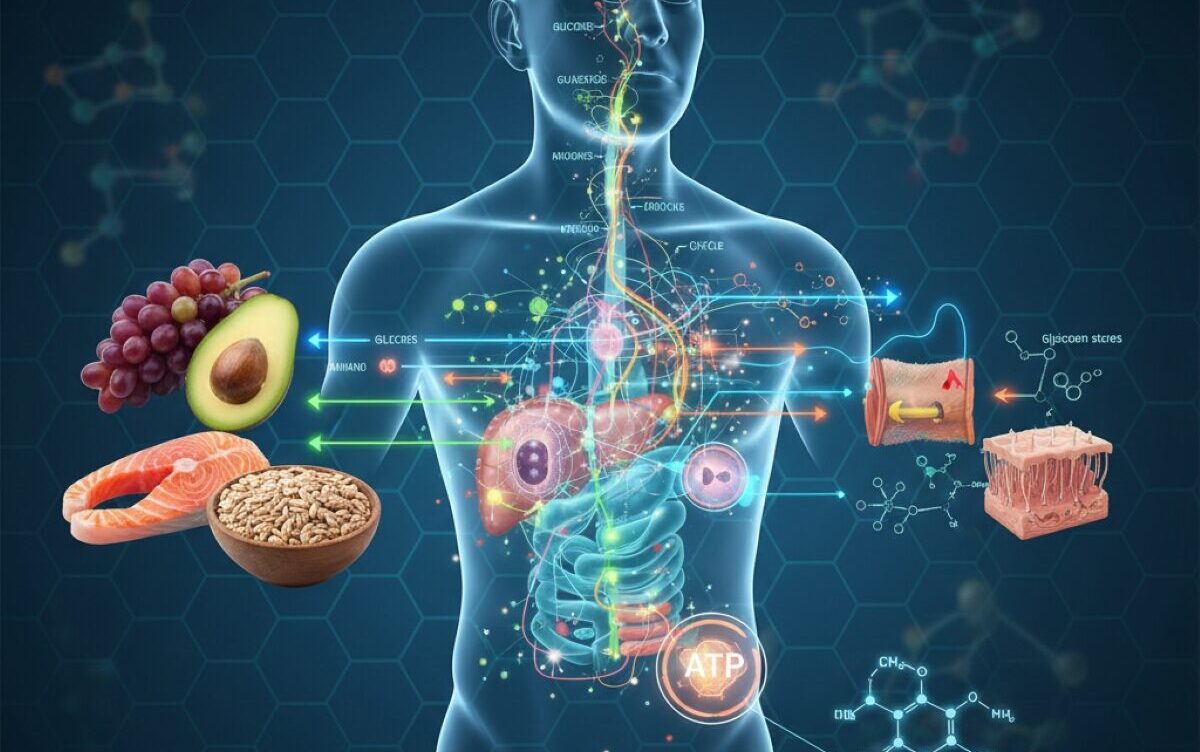
There is no single, clinically defined “Metabolic Reset Diet.” Instead, the term is used broadly to describe dietary programmes that claim to restore metabolic function by altering insulin signalling, fat oxidation, and hormonal regulation.
Common features across most metabolic reset approaches include:
- Significant reduction in refined carbohydrates and sugars
- Emphasis on whole foods, protein, and healthy fats
- Structured meal timing or fasting windows
- Short-term calorie restriction followed by “re-feeding” phases
- Claims of improving insulin sensitivity and fat burning
Some versions resemble low-carbohydrate or ketogenic diets, while others incorporate intermittent fasting, time-restricted eating, or cyclical calorie intake.
The central claim is that modern eating patterns keep insulin chronically elevated, suppress fat burning, and slow metabolic efficiency. A reset, proponents argue, allows the body to switch back to using fat as a primary fuel source.
The metabolic theory behind the reset
From a scientific standpoint, metabolism is not a switch that can be flipped on or off. It is a complex system regulated by hormones, nervous system signalling, muscle mass, sleep, stress, genetics, and long-term dietary patterns.
That said, several concepts used in metabolic reset diets are grounded in real physiology:
Insulin sensitivity
Reducing frequent glucose spikes can improve insulin responsiveness, particularly in people with insulin resistance or early metabolic dysfunction.
Metabolic flexibility
The ability to switch between carbohydrate and fat oxidation is impaired in obesity and type 2 diabetes. Certain dietary patterns can improve this flexibility.
Energy balance adaptation
Chronic dieting can reduce resting energy expenditure. Strategic periods of higher intake may help mitigate this effect, though evidence is mixed.
Where the reset concept becomes problematic is in suggesting that metabolism is “broken” and can be permanently fixed in a short time frame.
The potential benefits
For some individuals, metabolic reset diets may deliver short-term improvements, particularly when compared with highly processed, high-sugar eating patterns.
Improved blood sugar control
Reducing refined carbohydrates and snacking frequency can lower fasting glucose and insulin levels, especially in people with prediabetes.
Initial weight loss
Early weight reduction is common, driven by calorie reduction, glycogen depletion, and water loss. Fat loss may follow if the approach is sustained.
Increased dietary awareness
Many programmes encourage whole foods, protein intake, and mindful eating, which can improve overall nutritional quality.
Appetite regulation
Higher protein and fat intake can improve satiety for some individuals, reducing constant hunger and cravings.
These effects explain why metabolic reset diets often feel effective in the early weeks.
The downsides and limitations
Despite the appeal, there are important drawbacks that are often underplayed.
The “reset” is temporary
Metabolism adapts continuously. Once normal eating patterns resume, insulin levels, appetite signals, and energy balance often revert unless deeper behavioural changes are made.
Risk of metabolic slowdown
Aggressive calorie restriction can reduce resting metabolic rate, especially when muscle mass is lost.
Hormonal disruption
Very low-calorie or restrictive diets can negatively affect thyroid hormones, reproductive hormones, and stress hormones, particularly in women.
Not suitable for everyone
People with eating disorders, certain endocrine conditions, or high physical training loads may experience worsening health or performance.
Over-simplification of obesity biology
Obesity and metabolic disease are influenced by genetics, sleep, stress, medications, gut microbiota, and environment. Diet alone rarely explains outcomes.
The “inside track”: what clinicians and researchers actually focus on
Among metabolic researchers and clinicians, the emphasis has shifted away from short-term resets toward long-term metabolic restoration.
Key evidence-based priorities include:
- Preserving or increasing lean muscle mass
- Improving insulin sensitivity through consistent habits, not extremes
- Addressing sleep, stress, and circadian rhythm disruption
- Supporting sustainable dietary patterns rather than rigid protocols
From a clinical perspective, metabolism improves through stability, not shock.
This is why structured lifestyle interventions, resistance training, and gradual dietary changes outperform rapid resets in long-term studies.
The good
- Can interrupt highly processed eating patterns
- May improve metabolic markers in the short term
- Encourages whole foods and protein intake
- Can provide motivation and structure
The bad
- Often oversold as a permanent fix
- Risk of rebound weight gain
- May impair metabolism if overly restrictive
- Can promote diet cycling and metabolic stress
Where the concept fits today
The popularity of metabolic reset diets reflects a broader shift in how people think about metabolic health. There is growing awareness that calorie counting alone is insufficient, and that insulin resistance, inflammation, and hormonal regulation matter.
However, the science does not support the idea of a one-time reset that permanently repairs metabolism.
For individuals with metabolic dysfunction, the most effective strategies remain boring but powerful: consistent nutrition, resistance exercise, adequate sleep, stress regulation, and long-term adherence.
Bottom line
The Metabolic Reset Diet is less a defined scientific protocol and more a rebranding of familiar dietary strategies. While it may offer short-term benefits for some people, it should not be viewed as a metabolic cure or reboot.
True metabolic health is not reset. It is rebuilt, gradually and sustainably.
For those considering a metabolic reset approach, the key question should not be “How fast can I change my metabolism?” but rather “What can I maintain for the next five years?”
That answer, more than any reset, determines long-term metabolic health.
Metaboloic Myths that hold you back – https://lifesciencedaily.news/metabolic-myths-that-hold-you-back/