Alcohol problems are often framed as a failure of willpower or “poor lifestyle choices”. Yet clinical neuroscience has made that narrative increasingly untenable.
Problematic alcohol use is often a learned response to stress, a learned neurobiological adaptation, particularly when stress is chronic, early-life, traumatic, or socially entrenched.
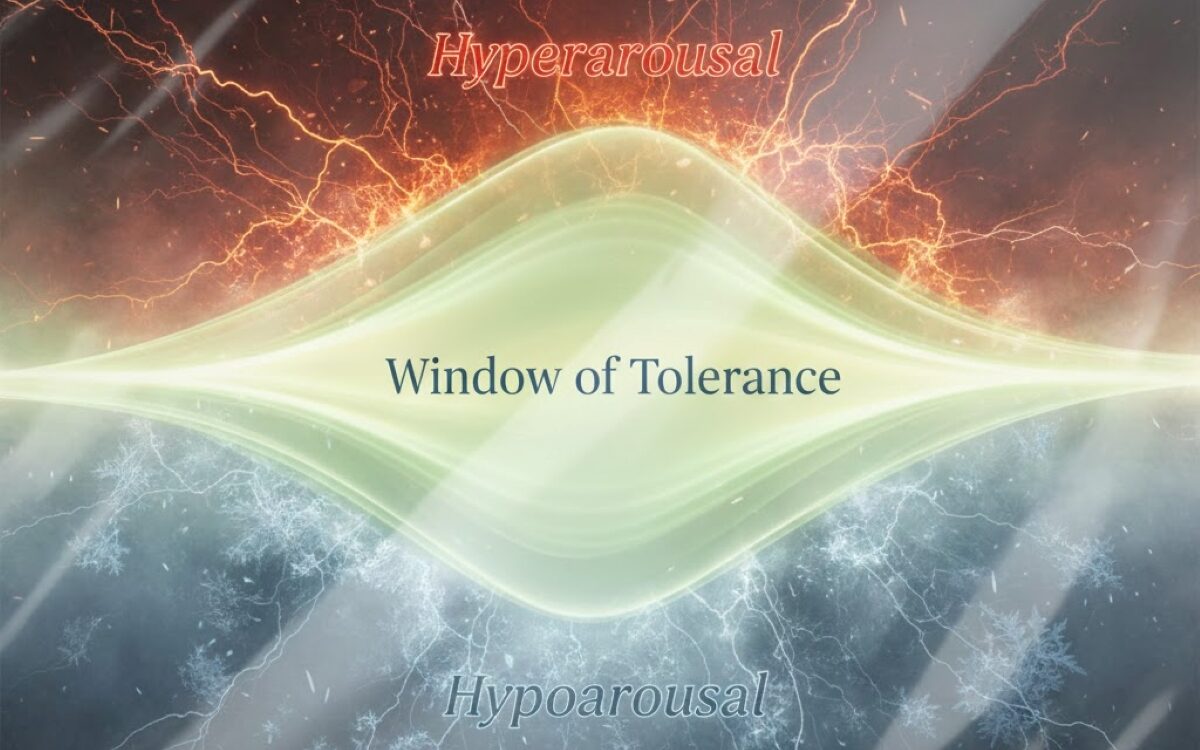
There are established links between trauma – particularly chronic or early-life interpersonal trauma – and neurobiological changes that alter how the nervous system detects and responds to threat. Chronic stress or trauma can lead to persistent hyperarousal, which is a prolonged “fight-or-flight” state. It can look like:
- racing thoughts
- agitation, irritability or anger
- a persistent sense of being unsafe
- panic symptoms (tight chest, fast heart rate)
- being “jumpy” or easily startled
- insomnia (or waking at 3–4am with adrenaline)
- being overly reactive to social cues, criticism or conflict
Hyperarousal is not always visible. Highly functioning professionals may appear composed externally, while internally like their nervous system is highly activated. Indeed, early experiences of rejection, criticism, shaming and neglect can lead to parts of the person striving, performing, working endlessly to prove worth and keep away from the pain of not feeling good enough.
Trauma can also lead to hypoarousal when the system shuts down, which is often associated with a “freeze” response. Hypoarousal can feel like:
- emotional numbness (“I don’t feel anything”)
- brain fog and difficulty concentrating
- detachment from self (“I’m not really here”)
- dissociation (time loss, unreality)
- fatigue or collapse
- social withdrawal
- a sense of emptiness or “deadness”
Hypoarousal is frequently perceived as low motivation or “not trying”. In reality, it’s a deeply biological protective state, when the nervous system has decided that feeling less is safer.
These adaptations were once likely very helpful. For example, being hyper-alert to the mood or behaviour of an unpredictable or aggressive parent would have helped the child to try to obtain safety more quickly. Working hard to be “good’ or gain approval was also once likely helpful. Similarly, detachment from the self during an aggressive act would have protected the child from the physical and emotional pain.
However, overtime an individual’s “window of tolerance” narrows, making stress responses both more easily triggered and slower to return to baseline. Whilst at the same time, parts of us get stuck in habitual striving, proving, performing responses without any adequate easy to down tool, switch gears or relax.
Alcohol as self-medication: Not just metaphor, but mechanism
The “self-medication hypothesis” fits with what we know about brain function. Alcohol reduces anxiety and causes sedation by acting on GABA and glutamate systems in the brain, as well as influences dopamine-based reward pathways.
For individuals experiencing hyperarousal or parts that relentlessly work to prove worth and gain approval, the first experiences of alcohol may feel like a pharmacological relief – fast, reliable and a socially sanctioned way to switch gears or quieten the parts in overdrive.
Less discussed, but also clinically common, is alcohol being used to up-regulate or shift out of hypoarousal. When numb or shut down, alcohol can serve to shift the internal state out of collapse into feeling more energised and temporarily connected.
Both up-regulating and down-regulating create a “positive” association with the alcohol for the user.
The long-term cost: Alcohol worsens nervous system instability
The tragedy is that over time, alcohol tends to destabilise the exact systems it temporarily regulates, and leads to:
- Poorer quality sleep
- Increases in baseline anxiety
- Sensitised stress pathways
- Greater mood volatility and irritability
- Lower distress tolerance
The nervous system recalibrates around alcohol, and over time, alcohol becomes a neuroadaptive requirement to return to “baseline”. Initial reward-driven use shifts into stress-driven use. Dependence is sustained less by pleasure than by the need to avoid withdrawal-associated dysphoria: anxiety, irritability, insomnia, autonomic instability, and emotional pain.
A way forward
In order to address the widespread issue of problematic drinking, it is important to understand that in many cases drinking is an attempt by a part of a person to solve an unresolved threat from earlier life. Often as an attempt to create balance internally.
Which is why alcohol treatment and relapse prevention approaches that focus only on removing alcohol can fail, because they remove the coping mechanism without offering alternative regulatory options or providing the trauma therapy needed to ease the underlying nervous system activation.
Hence why, rather than asking the question “why do they keep drinking?”, we should be asking “what unbearable states does alcohol temporarily relieve for them”?
Trauma-informed care can’t be an optional extra; it is mechanistically aligned with addiction biology. Comprehensive treatment would therefore integrate:
- teaching nervous systems how to come down from threat (behavioural, somatic and pharmacological)
- trauma therapy access
- social re-integration
When services insist on sequential treatment (“stop drinking first, then we’ll treat the trauma”), they risk removing the person’s primary coping mechanism while leaving the core drivers untouched—creating predictable relapse cycles, disengagement and reinforcing feelings of failure and shame.
Whereas Internal Family Systems (IFS) is a therapeutic model that views every human being as a system of protective and wounded inner parts, and works to help people address and heal these wounded parts of themselves. By addressing these parts, they can answer very important questions for themselves, such as:
- What is my relationship to alcohol?
- When did patterns of alcohol abuse or overconsumption begin?
- Does drinking serve me?
New services, such as Nul, have integrated IFS and other therapeutic or pharmacological methods to addressing cravings and alcohol dependence gradually, allowing people to reduce their drinking in a sustainable manner.

Dr Zandra Bamford, Consultant Clinical Psychologist and IFS Therapy Specialist at Nul