A New Energy-Centered Model of Metabolic Disease
For decades, sugar has been framed as a problem of excess. Too many calories. Too many insulin spikes. Too much sweetness in the modern diet. That framing has shaped public health guidance, food reformulation, and pharmaceuticals.
And yet, metabolic disease continues to rise.
In some populations, sugar intake has plateaued or declined. Artificial sweeteners have replaced sugar in many products. Powerful appetite-suppressing drugs are now widely prescribed. Still, rates of obesity, type 2 diabetes, fatty liver disease, cardiovascular disease, kidney disease, and neurodegenerative conditions continue to climb. That contradiction has pushed researchers to ask a deeper question:
What if sugar’s role in metabolic disease has been underestimated, not because we blamed it too much, but because we blamed it in the wrong way?
A growing body of research may suggest that sugar, particularly its fructose component, may exert its most important effects not through calories or insulin alone, but through cellular energy processing. This shift is giving rise to an emerging energy-centered model of metabolic dysfunction, one that sits upstream of calories, hormones, and behavior.
Moving Beyond Calories, Insulin, and Appetite Suppression
Calories and insulin dominate metabolic thinking for good reason. Energy balance matters. Insulin regulates fuel storage and use. More recently, glucagon-like peptide-1 (GLP-1) receptor agonists have produced dramatic weight loss by suppressing appetite and slowing gastric emptying.
These therapies are effective while they are used, largely because they reduce pressure on an already metabolically fragile system. But longitudinal data show a familiar pattern: most weight is regained within one to two years after discontinuation. Appetite returns. Cravings intensify.
What these approaches share is that they primarily treat downstream symptoms. They reduce intake or alter signaling, but leave key questions unanswered. Why do appetite and energy-conservation signals persist despite abundant fuel? And is insulin resistance truly a cause of disease, or an adaptive response to cells already operating at their energetic limit?
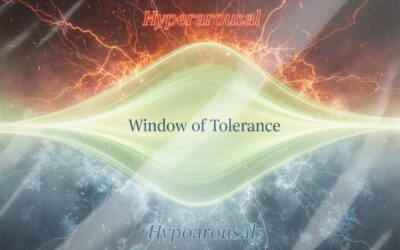
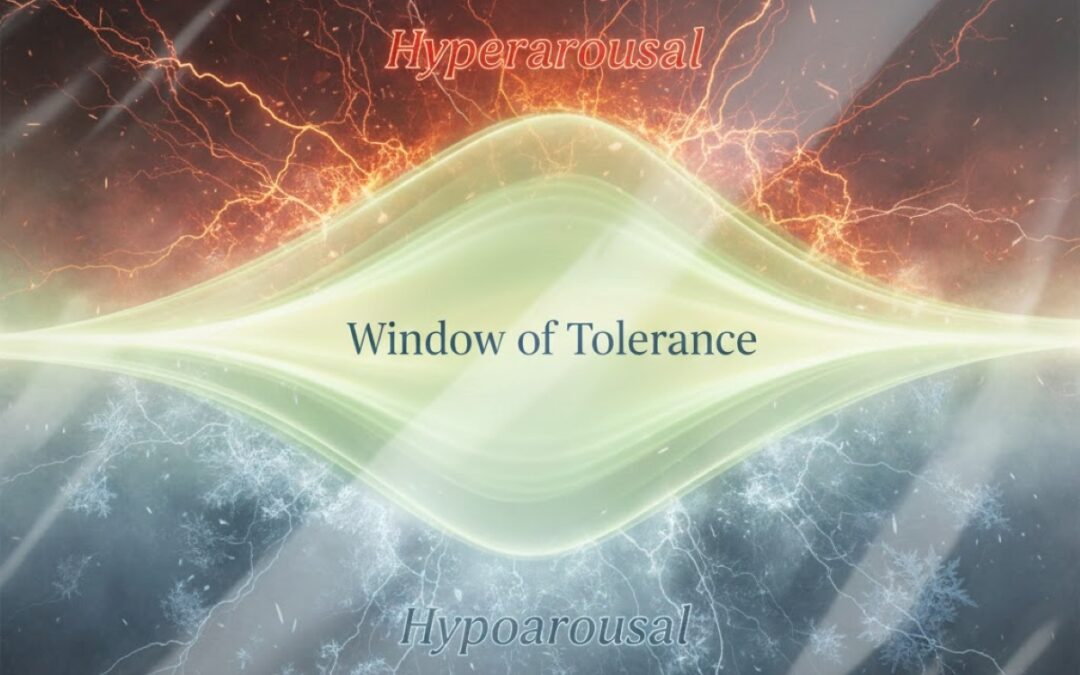
An energy-centered model reframes the problem. Instead of asking how much fuel enters the system, it asks whether fuel input and energy output are still properly matched at the cellular level, or whether an energetic bottleneck has formed.
Sugar, Fructose, and the Energetic Bottleneck
At a biochemical level, “sugar” is not a single entity. Table sugar (sucrose) is composed of equal parts glucose and fructose. High-fructose corn syrup (HFCS), common in processed foods, contains a similar ratio.
The distinction matters because glucose and fructose are handled very differently.
Glucose metabolism is tightly regulated and directly supports ATP production, the cell’s primary energy currency. Fructose metabolism bypasses key regulatory steps and initially consumes ATP before downstream energy production occurs.
Fructose acts as a survival signal. It promotes energy conservation, fat storage, and reduced metabolic rate, traits that would have aided survival during scarcity.
Problems arise when fructose exposure becomes chronic rather than episodic.
Under sustained exposure, cellular ATP levels fall, mitochondrial stress rises, and inflammatory signaling increases. Rather than increasing usable energy, cells enter a low-energy defensive state. Crucially, this is experienced not as energy excess, but as insufficient energy at the cellular level, even when calories are abundant.
Why Cravings and Insulin Resistance Rise Together
One of the most puzzling features of metabolic disease is that appetite and cravings often intensify as metabolic health worsens. This is commonly framed as a failure of willpower or hormonal control. An energy-centered model offers a clearer explanation, supported by biochemistry and preclinical research.
When cells struggle to generate usable energy, the body interprets this as an internal energy deficit. The logical response is to drive increased consumption, particularly of fast, rewarding fuels.
Cravings, in this context, are not irrational. They are predictable signals generated by energy-constrained cells attempting to correct a shortfall.
At the same time, insulin resistance emerges as a protective adaptation, not a malfunction. If cells are already operating near their energetic limit, allowing unrestricted fuel entry would worsen oxidative stress and cellular damage, much like flooding an engine that can no longer efficiently convert fuel into motion. By reducing insulin sensitivity, cells limit further substrate inflow and protect an already strained energy system.
Cravings and insulin resistance, then, are not root causes. They are downstream responses to an underlying energy bottleneck.
Sugar’s Reach Beyond Sweet Foods
Sugar’s influence extends far beyond obvious sweets.
Fructose can be produced inside the body itself. Under common stress conditions, glucose is converted into fructose within tissues via endogenous pathways.
Triggers include chronically elevated blood glucose, dehydration, high salt intake, alcohol exposure, and tissue hypoxia. This helps explain why many “cheat” foods and lifestyle stressors appear metabolically harmful despite not tasting sweet. They all pull on the same internal lever.
In this light, sugar is not just a dietary ingredient. It is a metabolic switch, persistently activated across the modern diet.
A Brief Word on Fruit
Any discussion of fructose raises the obvious question: what about fruit?
Fructose isn’t toxic. The issue is that fructose metabolism is relatively unregulated, so speed and load matter. A slow trickle is one thing. A fast, repeated flood is another.
Whole fruit is usually a slow trickle. It comes packaged with natural limiters, fiber, water, chewing effort, and plant compounds that slow absorption and buffer metabolic load.
Fruit also makes sense ecologically. Many plants use sweetness as a signal for seed dispersal. Symbiotically, animals respond by eating fruit aggressively before scarcity, gaining weight at exactly the moment it improves survival. That’s a seasonal switch, briefly flipped, then turned off.
The modern problem isn’t fruit in isolation. It’s continuous, year-round activation of a short-term survival pathway, without the natural brakes and buffering mechanisms that once kept both frequency and load in check.
Fragile Cells, Fragile Systems
Not all tissues respond equally to chronic energy stress. Organs with high metabolic demand are particularly vulnerable.
The liver, as the primary site of fructose metabolism, often shows early dysfunction. The kidneys, especially energy-intensive tubular cells, are highly sensitive to fructose-driven stress. Emerging research also implicates the brain, where even subtle impairments in energy handling can affect cognition and behavior.
Across these systems, a common pattern emerges. Cells exposed to chronic energy stress become fragile long before overt disease appears. Repair slows. Resilience declines. This energetic signature is detectable well upstream of diagnosis and scales predictably into clinical disease.
Why Interventions Plateau
Dietary strategies that sharply reduce fructose exposure, such as ketogenic diets, often produce striking improvements. By removing dietary fructose and minimizing glucose loads that drive endogenous fructose production, they reduce pressure on an already constrained system.
But lifelong restriction is difficult, and for many unrealistic. When pressure returns, cravings and weight regain often follow.
Unless cellular energy processing itself is restored, improvements tend to plateau.
A Forward-Looking Shift
The most important implication of this model is not a specific treatment recommendation, but a shift in research priorities.
Instead of focusing only on intake and signaling, researchers are asking how cellular energy capacity can be restored.
Support for this view comes from a rare genetic condition known as essential fructosuria, in which individuals cannot effectively metabolize fructose. Remarkably, the condition is benign. Despite lifelong fructose exposure, affected individuals do not develop typical features of metabolic disease.
This natural experiment suggests that fructose itself is not inherently toxic. Rather, it is the act of metabolizing fructose that drives downstream energy stress.
Preclinical research reinforces this idea. In animal models, disrupting fructose metabolism prevents fatty liver even when alcohol is force-fed, reverses Alzheimer-like pathology, reduces inflammation, and normalizes reward-seeking behavior.
Early-phase human studies and randomized trials are now beginning to test whether targeting fructose metabolism can translate into measurable benefits in people. One area of growing interest involves luteolin, a naturally occurring flavonoid found in plants such as parsley, thyme, and chamomile, which has been identified in preclinical research as an inhibitor of fructose metabolism. In a placebo-controlled study, a luteolin-containing formulation was associated with meaningful improvements in insulin sensitivity and reductions in liver fat, supporting the broader hypothesis that fructose metabolism itself may represent a modifiable upstream driver of metabolic dysfunction.
Alongside these trials, observational data involving liposomal luteolin point in the same direction. Many individuals report reduced cravings for sugar, refined carbohydrates, and alcohol, improved mental clarity, and greater metabolic stability.
Much more research is needed. But the implications are significant.
Rather than suppressing appetite from the top down, as weight-loss drugs do by overriding hunger and slowing intake without correcting the underlying defect, this approach targets metabolism from the bottom up, by addressing the energetic failure that drives cravings, insulin resistance, and relapse.
If this model continues to be validated, its implications extend far beyond weight and glucose control. It reframes chronic disease itself as a failure of cellular energy, a shared energetic signature that appears long before diagnosis and persists across metabolic, cognitive, vascular, and even oncologic conditions. The consistency of this pattern demands rigorous pressure-testing by researchers worldwide. If borne out, it suggests not a collection of disconnected diseases, but a common energetic failure with the potential for a unifying, system-level solution.
Author Bio
Chris Mearns is a metabolic health researcher and founder of LIV3 Health, where his work focuses on upstream, energy-centered models of metabolic dysfunction. His research explores how modern dietary and environmental stressors interact with conserved biological pathways to drive chronic disease, and has advised on translational strategies aimed at modulating fructose metabolism.