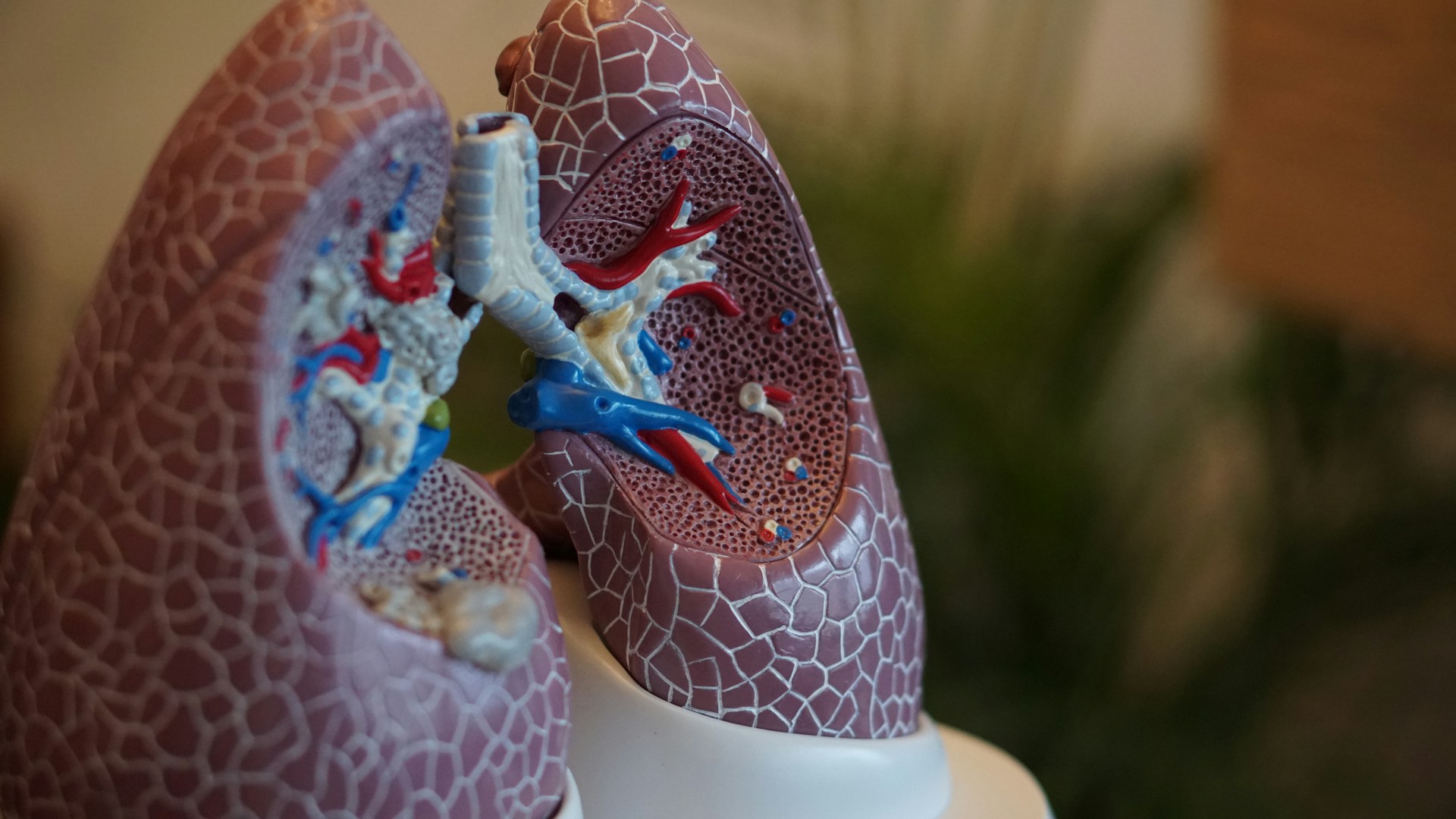
In a historic stride toward personalised cancer treatment, BioNTech—the German biotech giant behind one of the first COVID-19 mRNA vaccines—has launched the world’s first mRNA-based lung cancer vaccine, BNT116, into Phase I clinical trials across seven countries.
This groundbreaking effort marks a new chapter in cancer immunotherapy, leveraging lessons from the pandemic to target one of the deadliest forms of cancer: non-small cell lung cancer (NSCLC), which accounts for 85% of all lung cancer diagnoses worldwide.
A Vaccine—But Not for Prevention
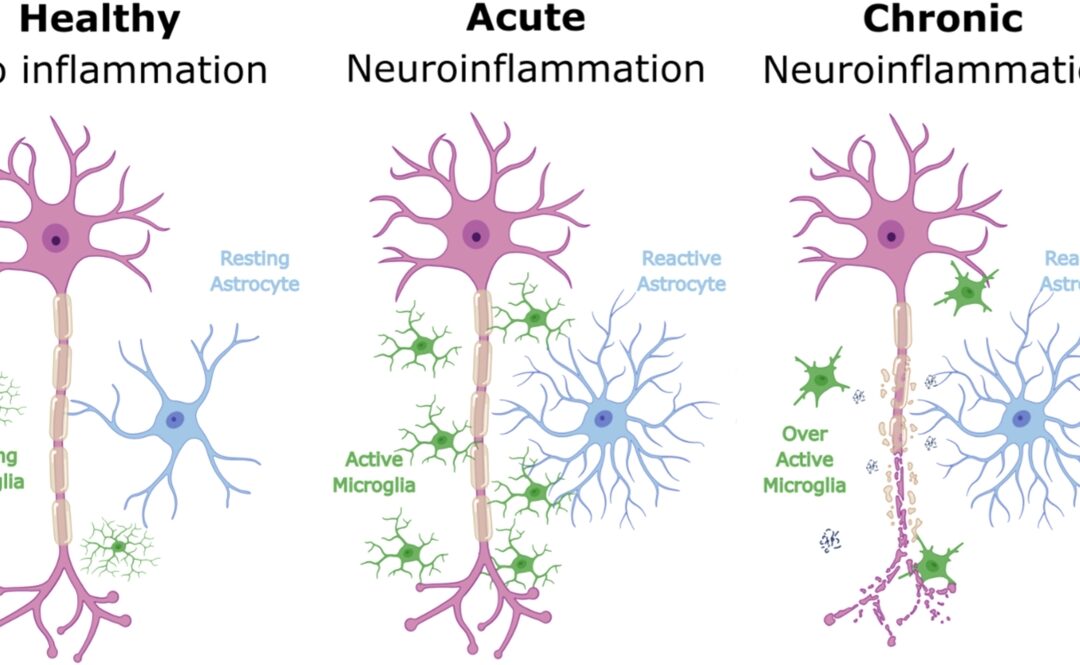
Unlike traditional vaccines designed to prevent disease, BNT116 is a therapeutic vaccine. Its mission? To stimulate the immune system to recognise and attack cancer cells that have already formed or are at risk of recurring after initial treatment.
Using mRNA technology, the vaccine encodes for tumour-associated antigens—specifically MAGE A3, PRAME, and CLDN6—proteins commonly expressed by NSCLC cells but not by healthy ones. Once administered, the patient’s body translates the mRNA into these antigens, effectively training T-cells to hunt down the cancer.
A Global Collaborative Trial
The Phase I trial is now recruiting patients in:
-
United Kingdom
-
United States
-
Germany
-
Spain
-
Poland
-
Hungary
-
Turkey
With 34 clinical research sites involved, the study will enrol around 130 patients diagnosed with early, advanced, or recurrent NSCLC. Participants will receive BNT116 either alone or in combination with existing immunotherapies to assess safety, immune response, and early signs of efficacy.
In August 2024, the first UK patient—a 67-year-old retired scientist from London—received a dose at University College London Hospitals (UCLH). Lead investigator Professor Siow Ming Lee described the moment as
“a very exciting new era of mRNA‑based immunotherapy.”
From Pandemic to Precision Medicine
The same mRNA platform that enabled rapid COVID-19 vaccine development is now powering a revolution in oncology. BioNTech, in particular, has doubled down on applying this technology to create individualized cancer therapies. BNT116 joins a growing pipeline of mRNA cancer vaccines targeting melanoma, pancreatic cancer, and colorectal tumors.
What sets mRNA cancer vaccines apart is their customisability and precision. Rather than relying on generic drug mechanisms, mRNA can be programmed to encode for patient-specific tumour markers—unlocking new potential for targeted immunotherapies with fewer side effects.
What Researchers Are Watching
The primary goals of this early-phase trial include:
-
Evaluating safety and tolerability
-
Measuring immune system activation, particularly T-cell responses
-
Tracking tumor response, recurrence, and patient survival over time
While results are still months away, early indicators could shape the next phases of development. If successful, BNT116 would move into larger-scale Phase II and III trials—paving the way for regulatory approval and broader patient access.
What’s Next?
Lung cancer remains the leading cause of cancer-related death globally, claiming over 1.8 million lives each year. Conventional treatments like chemotherapy and radiation often offer limited long-term benefit, especially in later stages of the disease.
mRNA-based therapies like BNT116 could shift the paradigm, transforming cancer from a life-threatening condition into a manageable chronic illness—or even eliminating it entirely in early-stage patients.
Meanwhile, researchers in the UK, including teams at Oxford and the Francis Crick Institute, are developing preventive lung cancer vaccines (like “LungVax”) targeting high-risk populations such as smokers and those with occupational exposure.
A Hopeful Horizon
While it’s still early days for BNT116, its launch into human trials represents a major step forward in the fight against cancer. By marrying cutting-edge mRNA science with global collaboration, researchers are edging closer to a future where cancer vaccines are not science fiction—but standard care.
As the world watches, this pioneering trial offers not just data, but hope—hope that one of the deadliest cancers may one day meet its match through innovation and immune precision.