In a pioneering medical achievement, a 25-year-old woman in China has become the first person in the world to reverse Type 1 diabetes using stem cells derived from her own body. The groundbreaking study, published in Cell in September 2024, marks a turning point in regenerative medicine and diabetes treatment—and offers a glimpse into a future where insulin injections may no longer be necessary.
The patient had lived with Type 1 diabetes for over a decade, reliant on daily insulin therapy to control her blood sugar. She had also undergone a previous liver transplant, which meant she was already on immunosuppressant medication—an important detail that helped set the stage for what was to come.
Researchers from Peking University and Tianjin First Central Hospital extracted fat tissue from the woman and chemically reprogrammed the cells into what are known as chemically induced pluripotent stem cells, or CiPSCs. These stem cells were then transformed into islet-like clusters—cells that can produce insulin, similar to those found in a healthy pancreas.
Instead of implanting the cells into the liver, as is typical in some clinical trials, doctors opted for a novel approach: placing the clusters in the abdominal muscle. This site allowed them to monitor the grafts more easily using MRI and, if needed, remove them safely. This decision turned out to be both effective and strategically sound.
Within just 75 days of the transplant, the woman no longer needed insulin injections. Over the course of the year-long follow-up, she maintained stable blood sugar levels, spending 98% of her time within the healthy range—a dramatic improvement from the 43% she had pre-transplant. Her HbA1c, a key indicator of long-term glucose control, dropped from 7.57% to 5.37%, reaching non-diabetic levels. More importantly, these results were sustained, with no signs of transplant rejection or autoimmune attack on the new cells.
The emotional impact was just as powerful. In interviews, the patient shared that she could now enjoy her favourite foods again—including hotpot, a popular dish often avoided by those with diabetes. “I can eat sugar now,” she said. “I enjoy eating everything.”
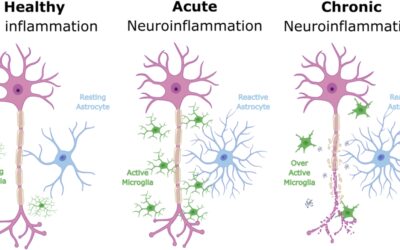
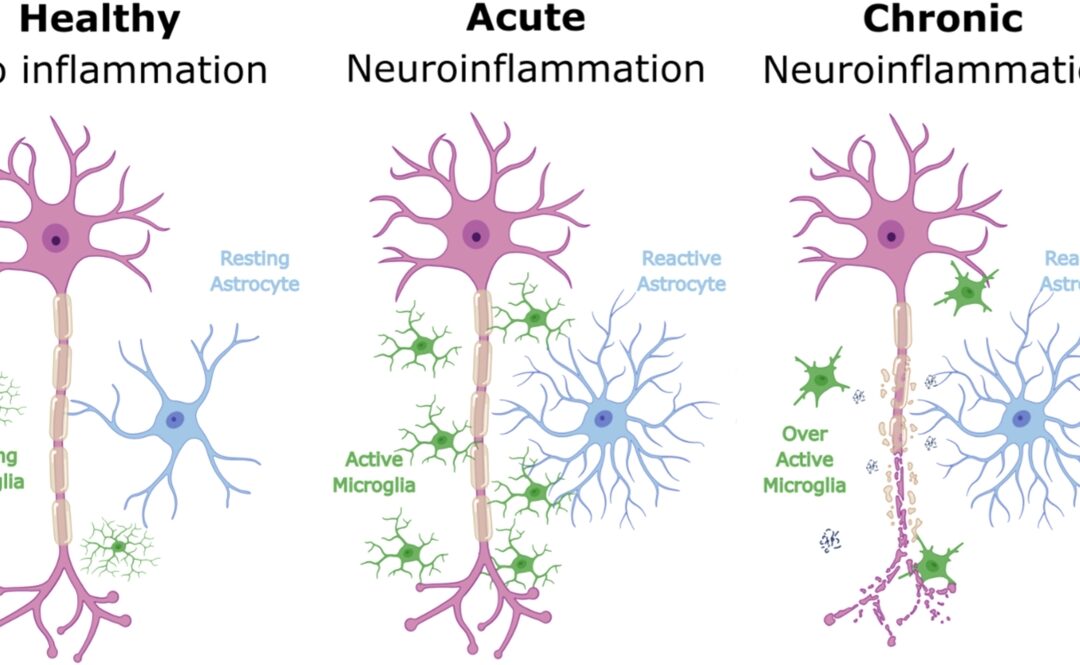
The scientific community has reacted with cautious optimism. Many experts describe the result as “remarkable” and “historic,” while also acknowledging the unique circumstances. Because the woman was already taking immunosuppressants due to her prior transplant, it’s unclear whether the same treatment would be successful in patients with an intact immune system. Type 1 diabetes is an autoimmune disease, meaning the body typically attacks insulin-producing cells—something researchers will have to address if the therapy is to be more broadly applied.
Still, the implications are enormous. This is the first time a patient’s own reprogrammed stem cells have been used to restore insulin production in Type 1 diabetes. The fact that the treatment did not involve donor cells also avoids the ethical and logistical complications of sourcing compatible tissues.
The trial, which includes two other participants whose results are not yet public, is ongoing. Scientists are now working to refine the approach, including methods to protect the new islet cells from immune attack without lifelong immunosuppression. Some strategies under development involve encapsulating the cells in protective biomaterials or engineering them to evade immune detection entirely.
Globally, other trials are exploring similar concepts with donor-derived or lab-grown islet cells, often with promising early results. One North American trial recently reported that ten out of twelve participants achieved insulin independence. However, this Chinese study is the first to use autologous stem cells—making it a milestone in personalised medicine.
While it’s too early to call this a cure, the success of this case opens up a new frontier in diabetes care. If replicated in larger, more diverse groups of patients, this kind of therapy could eventually free millions from the burdens of constant glucose monitoring and insulin injections.
For now, the world watches as one woman’s transformation from diabetic to insulin-free becomes a symbol of what science may soon make possible for many.