Spinal cord injuries remain one of the most challenging conditions in modern medicine. Damage to the spinal cord often leads to permanent paralysis, loss of sensation, and a dramatic decline in quality of life. For decades, treatment options have been limited to rehabilitation and symptom management, with little hope of true neural repair. Recent work in Japan, however, may signal a turning point.
A pioneering clinical study led by researchers at Keio University has demonstrated promising early results using induced pluripotent stem cells (iPSCs) to repair spinal cord injuries. This approach represents one of the most advanced applications of regenerative medicine to date.
From Ordinary Cells to Neural Repair
Induced pluripotent stem cells are created by reprogramming ordinary adult cells such as skin or blood cells back into a stem cell like state. These cells regain the ability to differentiate into multiple specialized cell types. In this study, iPSCs were carefully guided to become neural progenitor cells, capable of supporting nerve regeneration and restoring neural connections.
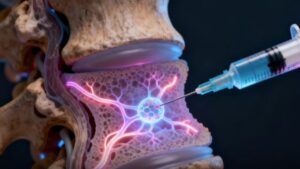
Within the first weeks following traumatic spinal cord injury, approximately two million of these reprogrammed cells were transplanted directly into the damaged region of the spinal cord. The timing was critical: the early post-injury phase provides a window in which inflammation can be managed and regenerative signals are still active.
Encouraging Early Outcomes
The early clinical outcomes have been cautiously optimistic. Some patients demonstrated partial recovery of sensory perception, improved muscle control, and in certain cases, the ability to stand or initiate stepping movements with support. While full recovery was not achieved, these functional gains represent meaningful progress in a condition historically considered irreversible.
Equally important is the safety profile. During the first year of monitoring, clinicians reported no serious adverse effects, including no abnormal cell growth or tumor formation—a key concern in stem cell–based therapies. This one-year safety milestone is considered critical in evaluating the viability of iPSC-based treatments.
Why This Matters Scientifically
This study provides some of the first clinical evidence that iPSC-derived neural cells can survive, integrate, and contribute to functional improvement in the human spinal cord. Previous successes in animal models did not always translate to humans, making this trial especially significant.
From a mechanistic perspective, the transplanted cells are believed to:
- Support damaged neurons through trophic factors
- Promote remyelination of nerve fibers
- Help reconstruct disrupted neural circuits
Rather than replacing the spinal cord outright, the therapy appears to create a biological environment conducive to repair.
Still Experimental, But Transformative
Despite the excitement, researchers emphasize caution. The treatment remains experimental and has been tested on only a small number of patients. Larger, multi-center clinical trials are now being planned to validate efficacy, refine dosing, and determine which patient populations may benefit most.
Nevertheless, the implications are profound. If larger trials confirm these results, iPSC based therapies could become one of the most impactful breakthroughs in regenerative medicine offering hope to millions of people worldwide living with paralysis.
A Glimpse Into the Future of Regenerative Medicine
This work underscores a broader shift in medicine: moving from managing damage to actively repairing it. Japan’s leadership in iPSC research, supported by decades of foundational stem cell science, is now translating into real clinical potential.
While challenges remain, this study represents more than a medical experiment it is a glimpse into a future where devastating neural injuries may no longer be permanent.
For patients, clinicians, and scientists alike, the message is clear: regenerative medicine is no longer theoretical. It is beginning to reshape what recovery can mean.
Author: Muhammet Furkan Bolakar
LinkedIn: Profile