After decades of promise and setbacks, advanced manufacturing platforms and robust Phase 2/3 trials are demonstrating whether MSCs can deliver transformative treatments for high-burden diseases
Mesenchymal stromal cells (MSCs) have been called the most promising therapy in regenerative medicine for over 20 years. Yet despite 1,900+ clinical trials initiated globally, commercial success has fallen short of expectations.
Why the disconnect between extraordinary preclinical promise and clinical reality?
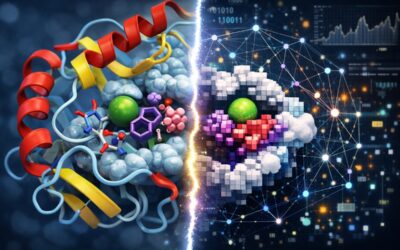
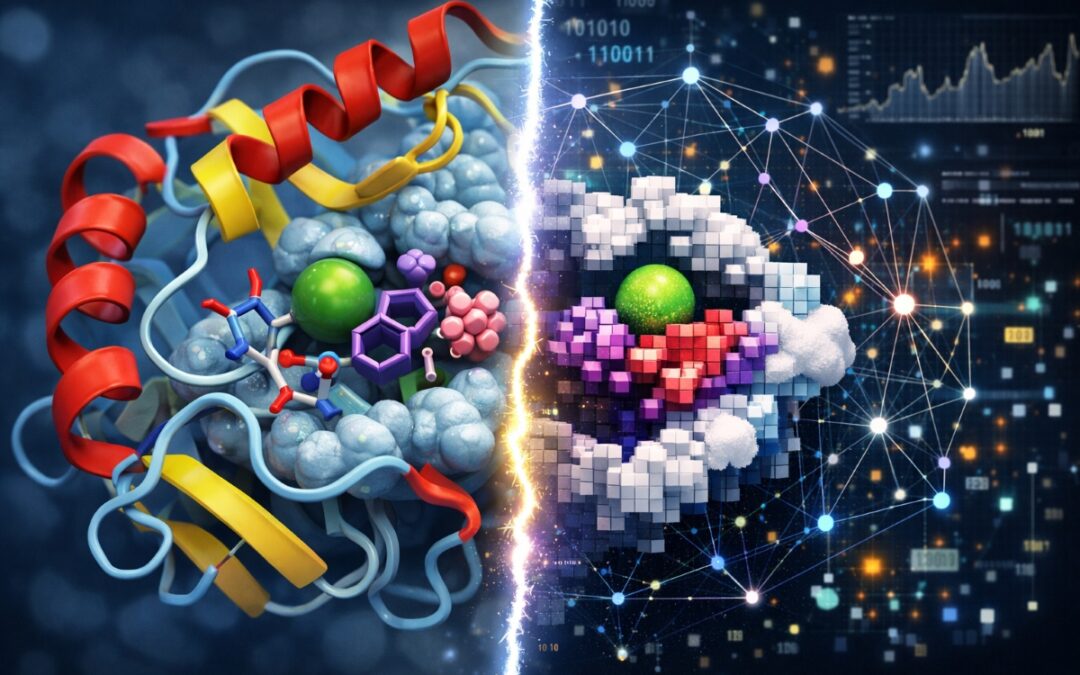
The answer lies not in the biology – MSCs’ immunomodulatory and regenerative properties are well-established – but in two fundamental challenges: manufacturing consistency and the rigorous clinical evidence required to bring any new therapy to market.
Today, with next generation manufacturing in place and rigorous efficacy trials reaching completion, we’re finally positioned to determine if MSC therapy can deliver for patients facing devastating diseases with limited treatment options.
The MSC promise and the manufacturing problem
MSCs possess unique therapeutic properties that make them attractive candidates for treating a wide range of conditions. Their ability to modulate immune responses, reduce inflammation, and promote tissue repair has driven investigation across diseases from graft-versus-host disease and osteoarthritis to respiratory failure and diabetes complications.
However, the field has been plagued by a fundamental manufacturing bottleneck. Traditional MSC production relies on harvesting cells from donated tissue such as bone marrow, adipose tissue, or placenta. This approach presents several critical challenges that have likely contributed to limited clinical success.
Firstly, donor-to-donor variability means that MSCs from different individuals behave differently, creating batch-to-batch inconsistency that makes it difficult to predict therapeutic outcomes.
Secondly, each tissue donation yields only a limited number of MSCs, requiring extensive culture expansion to generate sufficient cells for treatment. This prolonged expansion causes the cells to age prematurely and lose potency.
Lastly, the regulatory complexity of changing source material creates substantial commercial risk. When manufacturers switch to new donors, regulatory authorities require comparability testing to demonstrate that the new batches perform the same as those used in clinical trials. This is a costly and time-consuming process with no guarantee of success.
These manufacturing challenges have contributed to inconsistent clinical trial results and failed pivotal studies, even when the underlying biology suggested MSCs should be effective. The industry has increasingly recognised that manufacturing must evolve for the field to progress.
Our next-generation Cymerus™ platform, using induced pluripotent stem cell (iPSC) technology, addresses these limitations by providing an effectively unlimited supply of consistent MSCs from a single donor source, thus avoiding the problem of donor-to-donor variability. Furthermore, by harnessing scale at the starting material (iPSC) stage of the process, much fewer MSC population doublings are required compared to traditional methods. This provides a means of producing younger, more potent and consistent cells in an eminently scalable manner.
Clinical evidence is the only currency that matters
No amount of manufacturing innovation matters without clinical proof. Randomised, controlled, adequately powered trials are essential to demonstrate that new therapies are both safe and effective.
Proper trial design requires careful attention to multiple factors including appropriate endpoints that measure clinically meaningful outcomes, sufficient patient numbers to achieve statistical significance, and clinical evaluation in settings that reflect current standard of care. Only trials fulfilling these criteria can provide meaningful information on treatment safety and efficacy.
Perhaps unsurprisingly, the majority of MSC clinical trials to date have been small, uncontrolled studies that, while scientifically interesting, could not support regulatory approval or commercial development.
Today’s landscape shows a field that has learned from past challenges. We’re seeing larger, more rigorous trials being initiated across multiple indications, representing a significant maturation in both trial design and manufacturing approaches.
Addressing diseases with high unmet need
MSCs are being investigated in conditions where effective treatments remain desperately needed. Three examples illustrate both the promise and the challenge:
Acute graft-versus-host disease represents a devastating complication following haematopoietic stem cell transplantation or similar procedures, where donor immune cells attack the recipient’s tissues. Approximately 50% of patients don’t respond to first-line steroid treatment, and historical two-year survival rates in steroid-resistant patients are below 20%.
Despite the relatively small patient population – estimated at 20,000 cases annually – the unmet need drove the 2023 FDA approval of Ryoncil for paediatric steroid-resistant acute graft-versus-host disease, marking the first MSC therapy approved in the United States.
Osteoarthritis affects over 500 million people globally, yet current treatments only manage symptoms without altering disease progression. No disease-modifying therapies are currently approved. As the condition progresses, patients face increasingly limited mobility and often require joint replacement surgery. MSCs offer the potential to actually halt or reverse the degenerative process, representing a potential breakthrough in a multi-billion-dollar market.
Diabetic foot ulcers affect up to one-third of diabetes patients and represent the leading cause of non-traumatic amputation. Standard care often proves inadequate for these slow-healing wounds. Novel delivery methods, such as topical application of MSCs via wound dressings, are expanding the utility of cell therapy beyond traditional intravenous administration.
Diseases such as these are exactly where breakthrough therapies are most needed. And where regulators and health care practitioners are highly motivated to support effective new therapies through mechanisms like orphan drug designation and other regulatory benefits.
Proof points on the horizon
This year represents a potential inflection point for the MSC field. Two major efficacy trials are expected to report by the middle of 2026, which will shed further light on whether consistent, well-manufactured MSCs combined with robust trial design can deliver reproducible therapeutic benefits.
The stakes are high. If successful, we can expect rapid acceleration in pharmaceutical partnerships, expansion into additional indications, establishment of clearer regulatory pathways in multiple jurisdictions, and increased investment in next-generation MSC therapies.
Cynata’s nearly coinciding Phase 2 and Phase 3 readouts, both expected in the second quarter of 2026, position us at the forefront of this proving ground. Success in either indication would validate our platform and open pathways to partnerships and commercialisation. Success in both would demonstrate the broad applicability of our manufacturing approach across different disease mechanisms and delivery methods.
MSC therapy is finally moving from hype to hard science. The field has matured significantly thanks to next generation manufacturing combined with better trial design, leading to more robust data.
After decades of promise, we’re finally positioned to know whether MSCs can fulfill their therapeutic potential. Now we wait for the evidence that will hopefully transform medicine and patient outcomes globally.
Dr Kilian Kelly is CEO and Managing Director of Cynata Therapeutics, an ASX-listed clinical-stage biotechnology company developing MSC therapies using its proprietary Cymerus™ iPSC platform.