How AI and Biomarkers Are Accelerating the Fight Against Motor Neurone Disease
Every ninety minutes in the United Kingdom, someone receives a diagnosis of Motor Neurone Disease (MND), also known as Amyotrophic Lateral Sclerosis (ALS), and every ninety minutes, someone loses their life to it. This devastating neurodegenerative condition progressively destroys the nerve cells that control movement, speech and breathing. Despite decades of research, therapeutic options remain extremely limited and largely palliative.
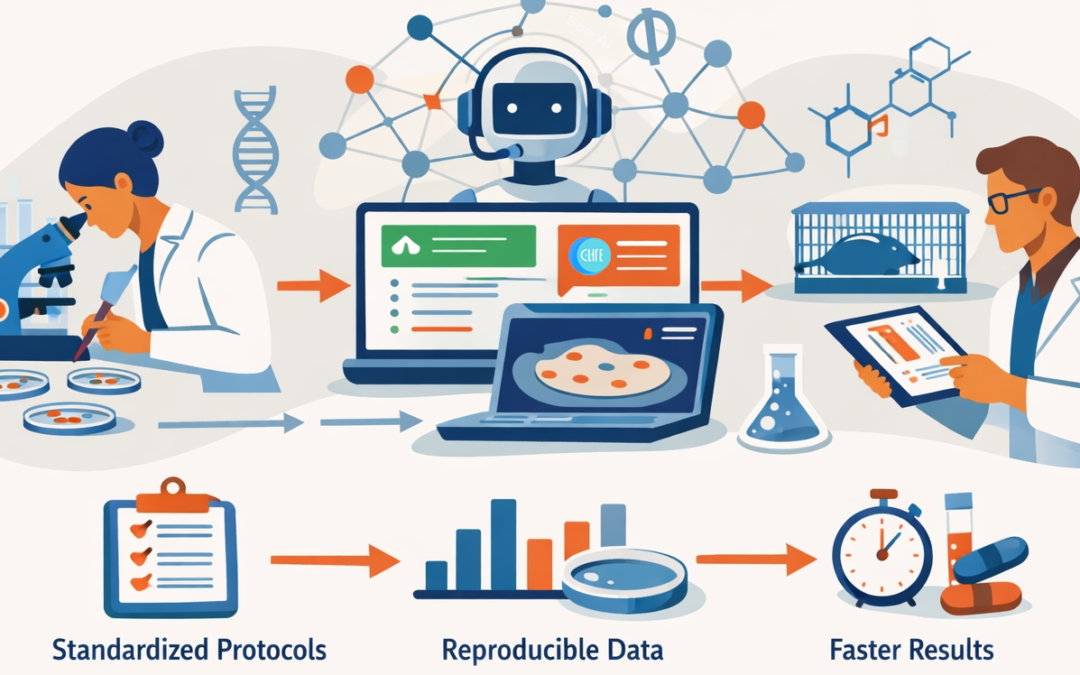
A new wave of innovation is beginning to change that reality. Advances in artificial intelligence (AI) and biomarker discovery are reshaping the MND research landscape, offering opportunities for earlier diagnosis, more adaptive trial design and personalised therapies. What was once a disease defined by uncertainty is now becoming a proving ground for data-driven progress across the life sciences.
The challenge: A disease that outpaces our tools
For people living with MND, time is critical, yet the journey to a confirmed diagnosis often takes between twelve and eighteen months. The symptoms frequently resemble other neurological disorders, and by the time a diagnosis is confirmed, motor neurones are already irreversibly damaged.
From a research and industry perspective, MND presents several interconnected challenges. The disease exhibits significant heterogeneity in its progression, limiting the ability to design efficient clinical trials. Small patient populations restrict statistical power. Preclinical models rarely reflect human disease biology accurately, and slow clinical endpoints delay understanding of therapeutic efficacy. These factors have led to numerous late-stage trial failures. Within the life sciences community, MND has long stood as an example of high unmet medical need paired with limited clinical success.
AI meets biomarkers: The convergence driving new discovery
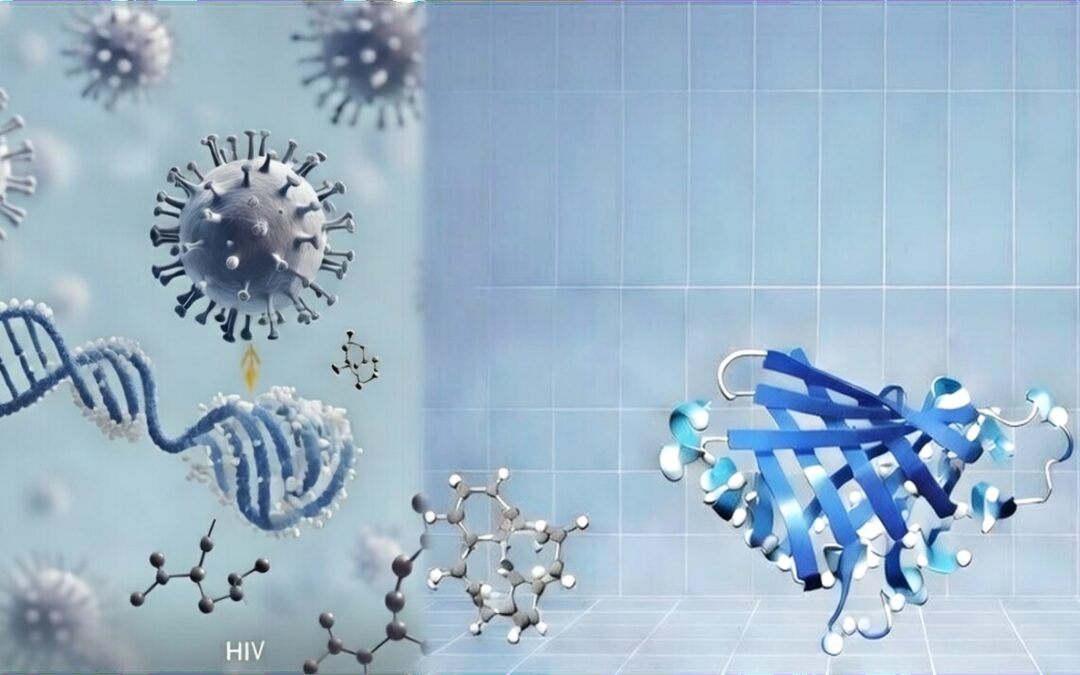
The next generation of MND research is emerging at the intersection of AI, data integration and biomarker science. AI excels at recognising complex, nonlinear patterns across large, multimodal datasets, which are typical of neurodegenerative disease research. Biomarkers, in turn, provide the biological anchors that turn these insights into clinically relevant outcomes.
One such biomarker, neurofilament light chain (NfL), a structural protein released during neuronal damage, has become a leading indicator in MND studies. Elevated NfL levels in blood or cerebrospinal fluid can signal early neuronal injury and predict the rate of disease progression. In the trial of Tofersen, marketed as QALSODY®, patients with a mutation in the SOD1 gene experienced a 40 to 50 per cent decrease in plasma NfL levels over six months, demonstrating its value as a measurable indicator of neurodegeneration. Integration of NfL data with genomics, imaging and digital health metrics is increasingly used to characterise disease subtypes and predict clinical outcomes.
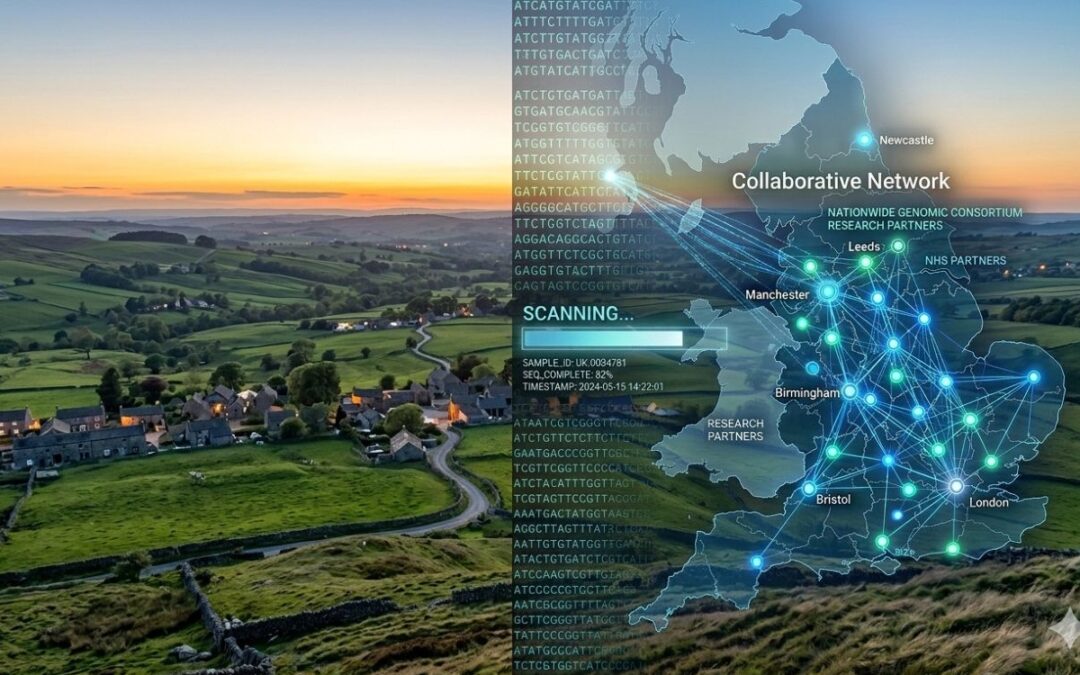
AI-powered analyses of digital biomarkers, such as speech and movement data collected from smartphones or wearable devices, can also detect subtle motor changes well before they become clinically apparent. This approach transforms routine patient monitoring into continuous data streams that support both research and care. In parallel, large-scale genetic initiatives such as Project MinE are mapping the genetic landscape of MND. Machine learning applied to Project MinE and related datasets has identified new genes associated with increased disease risk. Combined with proteomics and metabolomics data, these findings are providing a systems-level understanding of MND biology and building the foundations for precision therapeutics.
From bench to bedside: Rethinking clinical trials
One of the most immediate benefits of combining AI and biomarker research is the potential for faster and more efficient clinical trials. Traditionally, MND trials have required large patient cohorts and long observation periods to measure meaningful outcomes. AI now enables identification of optimal patient subgroups, modelling of disease trajectories and even simulation of control arms, reducing the recruitment burden. Adaptive platform trials, in which multiple therapies can be tested within a single framework, are also gaining momentum.
A major milestone was achieved with the accelerated approval of Tofersen (QALSODY®) in April 2023 for adults with SOD1-related ALS. The United States Food and Drug Administration (FDA) granted approval under its Accelerated Approval pathway based on evidence showing a reduction in plasma NfL levels, which the FDA deemed “reasonably likely” to predict clinical benefit. Continued approval will depend on confirmatory results from the ongoing Phase III ATLAS study.
In May 2024, the European Commission granted marketing authorisation for QALSODY® under exceptional circumstances, marking the first treatment in the European Union to target a genetic cause of ALS. This achievement validated the biomarker-driven development framework and set a precedent for innovation in rare neurodegenerative diseases.
Collaboration as the catalyst
Progress in MND research has always relied on collaboration. The complexity of the disease requires expertise from neurologists, data scientists, geneticists, clinicians and patient advocacy groups. The UK-based MND Association has championed projects that combine AI with large biobank and clinical datasets. In partnership with companies such as PrecisionLife, the association has helped identify new genetic risk factors for MND.
Public-private collaborations involving universities, biotechnology start-ups and major pharmaceutical companies are accelerating the translation of data into therapies. These partnerships are not only sharing information but are also changing the research culture. Instead of isolated studies, researchers are now embracing open science, cloud-based data analysis and AI-enabled workflows to accelerate progress from discovery to application.
A cross-disease ripple effect
The lessons learned from MND extend far beyond this single condition. Many of the cellular mechanisms uncovered in MND research, such as protein misfolding, mitochondrial dysfunction and RNA dysregulation, are also implicated in Alzheimer’s disease, Parkinson’s disease and frontotemporal dementia. The analytical tools developed to study MND biomarkers and AI-based modelling are already being used to advance research across these disorders, creating a shared ecosystem of discovery. MND, once regarded as an intractable challenge, may hold the key to breakthroughs across neurodegenerative medicine.
The human element: Turning data into hope
Despite the technological sophistication of these advances, progress in MND is ultimately about people. AI algorithms and biomarker tools are designed to deliver earlier diagnoses, improve care and, most importantly, extend quality of life. The next step is ensuring that these innovations move from the research setting into clinical practice. Achieving this will depend on open data standards, robust ethical frameworks for patient data use, sustainable investment in biomarker validation and long-term studies, and close collaboration between academia, industry and patient advocacy organisations. When these conditions align, the life sciences sector can not only innovate but also bring measurable benefit to patients.
Conclusion: Redefining what is possible
MND has long symbolised one of medicine’s most difficult frontiers. The convergence of AI and biomarker science is beginning to change that story. With each dataset analysed, biomarker validated and model refined, the field moves closer to predicting, slowing and eventually preventing neurodegeneration. For professionals across life sciences, from biopharma and diagnostics to digital health, MND represents both a challenge and an opportunity: to expand the boundaries of what science can achieve and to collaborate in ways that bring hope to patients. In the race against MND, innovation is not simply about technology; it is about time.